So you had what you thought was going to be a routine dental or medical evaluation and your provider has just informed you that you and/or your child has a breathing or airway issue. You are understandably confused and possibly have been given too much information about a problem you never knew existed.
You have landed in the right place! I will break down the logistics of some information you have been given, possibly give you more you didn’t think of and present you with a to-do list so you know how to proceed.
All was well and right with the world until that visit. You knew your body and/or your child and there were no words other than healthy to describe you. Yet, a few questions and one exam later knocked down all the blocks in the tower you were building.
Here’s what you should know:
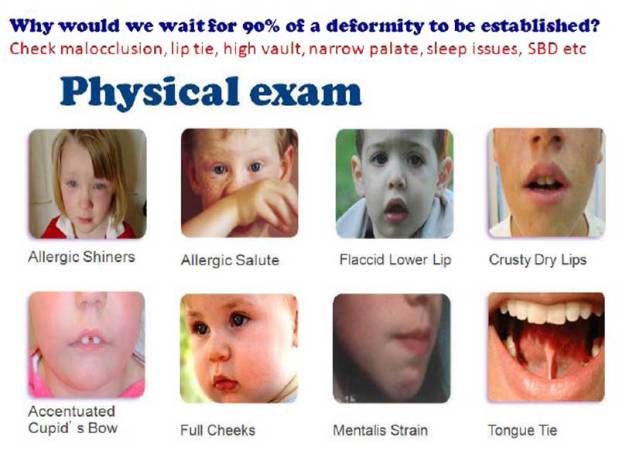
- Mouthbreathing is ineffective and inhibits your body from functioning optimally. The visible signs that your doctor may have noticed are in the graphic below. These are the tip of the iceberg in diagnostic signs of an orofacial myofunctional disorder (OMD).
- There is no official way to predict the future health implications of OMDs. Airway issues and dysfunctions have been tied to sleep apnea, asthma, eczema, TMJ disorders, ADHD/ADD, daytime sleepiness, tongue thrust, speech issues, enlarged tonsils/adenoids, snoring, grinding, messy/loud eating, picky eating, slow labored eating, poor dental arch formation, malaligned teeth, poor facial development, anxiety, poor emotional regulation, frequent congestion, and proneness to allergies.
- Not all tongue ties need to be released. There is a functional and non-functional tongue. The decision for a release should always include a myofunctional therapist, even if just for a consultation. Craniosacral therapists and Osteopathic physicians are also great to consult for eligibility to release. Read more about them below in part 2.
- We spend 1/3 of our lives sleeping and there is no more critical bodily process than breathing, yet medical and dental schools spend less than 10 hours studying both. With the exception of specialists, medical school graduates are mostly unaware of sleep disordered breathing and orofacial myofunctional disorders. In fact, in most cases where a knowledgeable dental provider indicates an OMD and the patient/parent goes back to their primary care physician, the physician will disregard or dismiss the issue.
- While there are many possible causative factors for OMDs, the only preventative measures that can be considered are to have newborns evaluated for lip and tongue tie, breastfeed for 1-2 years without regular bottle supplementation, do not introduce a pacifier or take away a pacifier at or before 6 months of age, do not introduce sippy cups, go from breast to regular cup or cup with straw, allow babies to have tummy time, limit baby sleeping in unnatural positioners (walker, rocker, swing, bouncer, carrier), and discourage thumb, finger, tongue or object sucking. The aforementioned measures can help reduce the risk of a child developing an OMD but is not guaranteed. Some hereditary, genetic and otherwise elusive factors are involved.
- You are not alone. Due to our diets, fast-paced society, and perceived norms many people have OMDs that are undiagnosed. Hard crunchy foods are not the integral part of the diet as it used to be. Caffeine is the stimulant used to power the body and keep it alert and awake, as opposed to adequate oxygenation and sleep. Snoring, painful breastfeeding and needing braces are all considered normal in society, as opposed to signs of airway problems. If you took a walk down a city street and watched carefully, it is a good prediction to say that 70% of the people you pass will have an open mouth and one or more other signs from the graphic above.
- There are solutions, but you have to be prepared and fully aware of the time and financial commitment that it will require. If you take your steps wisely, you may be able to get some financial help from both medical and dental insurance to help reduce costs in some areas.
Which leads us to
What on earth do you do with all this new information? How do you apply it and where do you go from here?
The detailed plan
- Assemble your team
- Dentist- A progressive dentist that specializes in sleep and/or airway dentistry. This dentist does all types of “typical” dental services such as examinations, fillings and preventative care. However, they also evaluate for tongue ties, airway obstruction, screen for sleep issues and utilize orthopedic or orthodontic appliances to expand the airway. They can offer you dental solutions for sleep problems.
- Sleep Physician- A sleep specialist can consult with you and determine your need for a sleep study. A sleep study is used to monitor your brain and vital activity while sleeping. The physician will read the results of the study and determine if there were episodes of obstructive breathing or poor sleep quality. In some cases, a sleep study that results in a diagnosis of obstructive sleep apnea can warrant your medical insurance to reimburse or pay for dental appliances to expand the airway. A specially trained dentist (general or pediatric) or an oral maxillofacial surgeon can perform releases of tongue or lip ties.
- Bodyworker- This team member can feel and manipulate tensions, pains, and dysfunctions in the body. An osteopath is a medical doctor that specialized in osteopathic medicine. These doctors are often recommended by dentists who utilize the orthodontic appliances. Alternatively, a craniosacral therapist works with the cranium, spine and pelvic area. They are certified professionals who have at least 2-3 years of training and clinical experience. Sometimes trained in orthodontic appliances, bodyworkers understand how to symmetrically balance the growth of the palate with the entire cranium. With tongue ties and other body restrictions or tensions, they may be able to perform treatments to alleviate the tension or manipulate the restriction. In most cases, neither of these professionals are covered by insurances but may qualify for out-of-network reimbursement.
- Myofunctional therapist- A myofunctional therapist or orofacial myologist is a speech-language pathologist, dental hygienist or dentist that has pursued additional education and training for the treatment of OMDs. This professional can work with patients to help them establish proper oral resting posture. They are also able to help eliminate noxious oral habits, such as thumb sucking, nail biting or prolonged pacifier use. These professionals are able to assess the functionality of a tongue frenum to determine if the tongue is functionally or non-functionally tied.
- ENT- An ear, nose, and throat doctor can evaluate the airway for obstructions. They will determine if the obstruction is capable of rehabilitation without surgical intervention.
- Make modifications accordingly
- Change the diet. Along this journey, various members of your team will inform you that gluten, dairy, processed foods, and sugar all increase body inflammation. If you have an airway obstruction, the first and easiest change to make is in the diet.
- Perform nasal hygiene. Just as you would brush your teeth daily, cleanse the nasal passages with a saline rinse daily.
- Try natural solutions. Nasal strips can help to open the nasal passages. Sleeping on your side can help you to breathe better. Eliminate sucking objects (bottles, sippy cups and pacifiers) for young children. Be aware of your mouth posture and close the lips comfortably together to consciously nasal breathe.
- Research, Research, RESEARCH
- Don’t take everything you hear from your professionals and hold onto it. Process the information internally, and add the wealth of information available online from various professionals. Remember, you are not alone. There are blogs from professionals (like this one), blogs from individuals who chronical their journeys, peer-reviewed journal articles and research available for you to review online.
Once you know more, you are able to not just do better, but also BE better. It is a long and hard journey, but there is significant light at the end of the tunnel. You are strong enough to complete this journey.
Continue to follow this blog for more helpful posts that may guide you along the way.


9 thoughts on “An airway issue has been identified…now what?”